Minimally Invasive Computer Navigated Robotic Knee Replacement
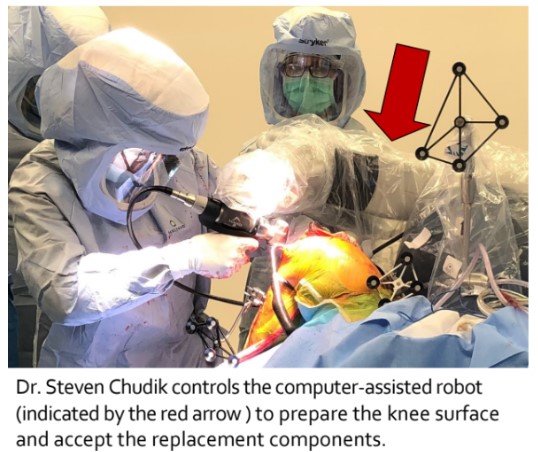
A board-certified, fellowship-trained orthopaedic knee surgeon and sports medicine specialist, Dr. Steven Chudik is renowned for his expertise and innovative procedures that reduce surgical trauma, speed recovery, and yield excellent outcomes.
Knee replacement surgery is a very successful orthopaedic procedure with reliable outcomes for patients with symptomatic, painful, and functionally limiting arthritis of their knee joints. Knee replacement surgery helps patients return to a functional ambulatory status with reduced pain which has an overall positive impact on the patient’s general health and quality of life. Studies on long-term survivorship for knee arthroplasty can be close to 100% at 10 years and remain just greater than 80% at 25 years.
Despite this promising data, not all patients obtain a satisfactory outcome, and innovation and new technology continue to push forward for better results and outcomes. Robotic-assisted surgical procedures are up and coming. Robotics have been used in multiple orthopedic subspecialties including spine, total joint arthroplasty, trauma, shoulder, and foot and ankle. Advantages in using robotic technology include the possibility of improving implant placement, balancing ligaments, limiting surgical exposures, better accessing difficult anatomic areas, decreasing x-ray use, and potentially reducing complications.
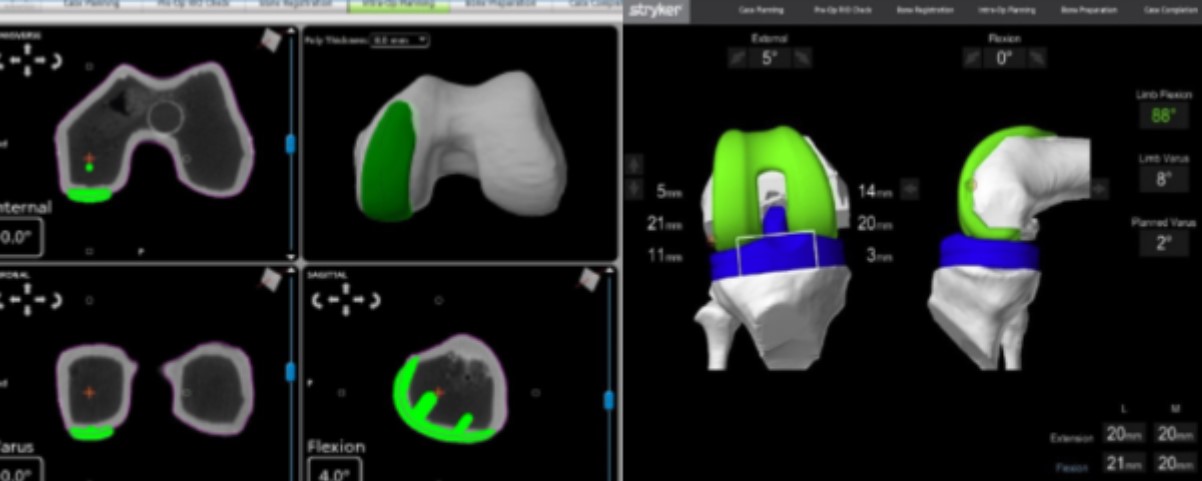
Robotic assisted procedures are still being studied and outcomes vary depending on the procedure and research available. Dr. Chudik performs computer navigated robotic-assisted total knee replacement surgery. Computer navigation with robotic assistance allows Dr. Chudik to plan and virtually perform the surgery on the computer even before making an incision. Pre-operatively, the patient is sent for a specialized computerized tomographic study (CT scan) of their extremity. The highly accurate anatomic CT scan data taken from the patient is loaded into a computer and processed with special software and a preliminary surgical plan is devised. Dr. Chudik can virtually perform the surgery on the computer and position the implants on the computerized images of the patient’s knee, determining the optimal size, position, and alignment of the knee replacement prosthetic implants.
Knee Replacement Expertise
- Arthritis, Non-Operative Treatment
- Unicompartmental Arthritis
- Total Knee Arthroplasty (Replacement) with Computer Navigation, Robotic Assistance
Individualized Treatment and Rehabilitation 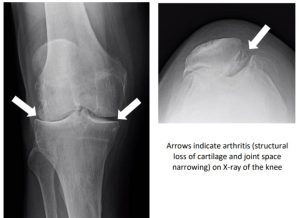
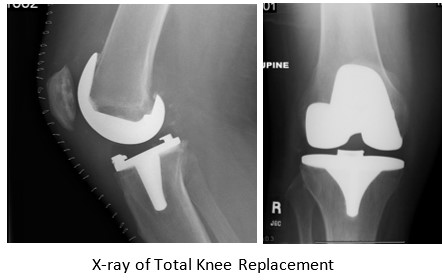
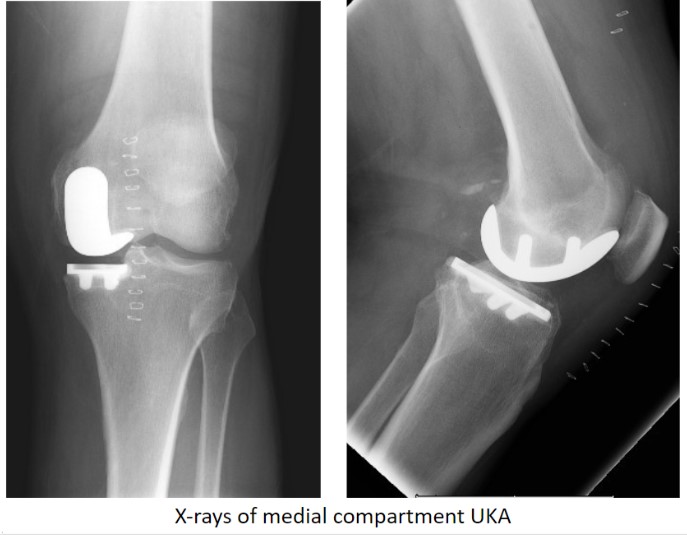
Total knee replacement surgery is indicated for patients with symptomatic knee arthritis who have failed conservative treatment. Knee arthritis is a painful and limiting condition that results from the structural loss of cartilage, the thin protective layer of firm but compressible tissue along the surface of the articulating (contacting) ends of our bones. Total knee replacement is performed by replacing that worn surface with a new artificial surface composed of metal and high molecular weight polyethylene (a fancy plastic). Outcomes from total knee replacement surgery depend upon how well the surgeon can position the implants to best restore the native anatomy, balance and tension the knee ligaments and allow normal kinematics (motion), all while minimizing surgical morbidity. To obtain the best implant position, function, and long-term outcomes and minimize surgical trauma, Dr. Chudik uses the latest state-of-the-art computer navigation technology with robot assistance to perform joint replacement surgery.
Frequently Asked Questions
- A robot-assisted knee replacement surgery is performed like traditional knee replacement surgery where Dr. Chudik replaces the damaged joint surface of your knee with a new artificial surface. The difference is that the assistance of a robot allows Dr. Chudik to balance and align the knee joint more precisely.
- Chudik will order a CT-scan of your knee with a specific protocol to obtain complex anatomic data to generate a 3-dimensional computerized knee joint model. Before surgery, Dr. Chudik performs a simulated surgery on the computer to make sure everything is precisely aligned and balanced on the computer. Then, later, Dr. Chudik conducts the surgery using the computerized plan and the robot, checking and measuring along the way to most precisely balance and align the knee.
- Patients who are candidates for traditional total knee replacement.
- Patients with knee arthritis and walking/standing limitations and intolerance.
- Patients with complex degeneration of the knee joint, deformities, post-traumatic arthritis, and arthritis from other causes.
- Enhanced surgical planning and precision with 3-dimensional imaging data, computer modeling, and robotic guidance.
- Optimal joint alignment and balance.
- Robotic knee replacement is not done by the robot alone. Instead, Dr. Chudik uses the robot to guide and improve implant placement.
- Chudik can plan and virtually perform the surgery on the computer before making any incision. This results in improved reliability and accuracy especially when addressing patients with more complex knee anatomy or deformities.
- The robot has safety controls that allow the surgeon to safely access less accessible areas through more limited approaches. This decreases the amount of surgery and tissue injury.
- There is also a potential reduction in complications.
- Most patients are discharged home on the day of surgery.
- Patients are allowed to weight bear as tolerated and walk immediately. Assistive devices like crutches or walker are used initially for comfort and balance.
- The surgical site must be kept clean and dry for the first 14 days after surgery. Showering lightly is allowed after two weeks but wounds cannot be submerged under water for three weeks.
- Return to driving my be delayed for up to four to six weeks following right knee surgery while awaiting return of sufficient motion and strength.
- Most patients return to sedentary work in about two weeks as long as the extremity can be elevated and there are no significant standing and walking requirements.
- Patients often attend physical therapy for up to three to four months to restore motion, strength, gait and function.
- Studies demonstrate that total knee replacement surgery has a positive impact on a patient’s general health and quality of life and nearly 100% of knee replacements are still surviving at 10 years and approximately 80% still at 25 years following the initial knee replacement surgery.
Testimonials and Patient Stories
Knee Anatomy
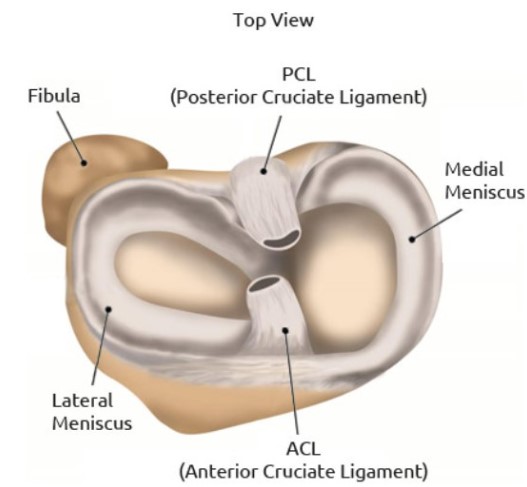
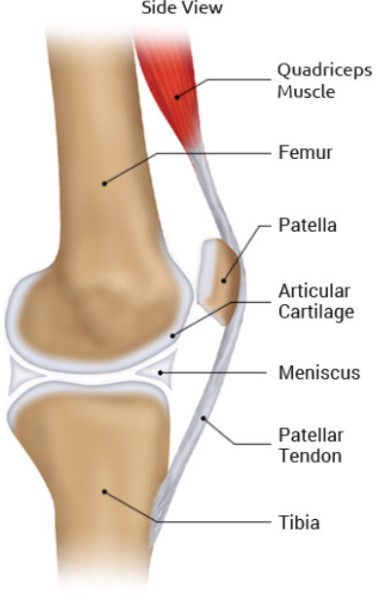
Your knees are the most commonly injured joints in your body. Unlike your shoulder that moves in all directions, your knees appear only to bend and straighten, but actually their movements are much more complex and involve rotation, translation, sliding and rolling.
Ligaments
There are four main ligaments connecting the bones at the knee joint and provide stability when you walk, run and jump. They are the:
- Anterior cruciate ligament (ACL)
- Posterior cruciate ligament (PCL)
- Medial collateral ligament (MCL)
- Posterolateral corner (PLC) ligaments including the lateral collateral ligament (LCL)
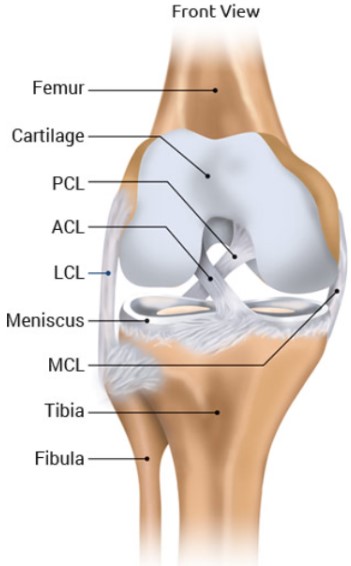
Cartilage and Meniscus
The joint surface of the knee is covered with a thin, but durable layer of cartilage over the ends of the femur, tibia, and patella and, along with the meniscus, allows the knee surfaces to articulate, move smoothly—almost frictionless and painlessly along each other. The cartilage lacks a blood supply and receives nutrition from the joint fluid. The meniscus has an unlimited blood supply. Without a blood supply and because of their relatively less active cellular makeup, the cartilage and meniscus do not maintain themselves. The cartilage and meniscus are extremely durable, but in time with “wear and tear” or following injury, they break down, fail, and lead to meniscus tears, cartilage damage, and eventually symptomatic (pain, stiffness, swelling) arthritis (failure of this protective joint surface).
Tendons and Muscles
Tendons also help provide knee joint stability and movement. They act like strong cables connecting your muscles to your bones. These muscle-tendon units cross joints to compress, hold and move joints in specific directions. Like other parts of your knee, they are susceptible to injury and overuse. The two knee tendons most commonly injured are the quadriceps and patellar tendons.
Injuries & Conditions
- Arthritis
- Patellofemoral Arthritis
- Unicompartmental Arthritis

Novel Surgical Procedures
- Total Knee Arthroplasty (Replacement) with Computer Navigation, Robotic Assistance
- Unicompartmental Knee Arthroplasty with Computer Navigation and Robotic Assistance
About Dr. Chudik

- Curriculum Vitae (CV)
- Video
- Website: stevenchudikmd.com
- Schedule an appointment online
- Email: contactus@chudikmd.com
- Phone: 630-324-0402
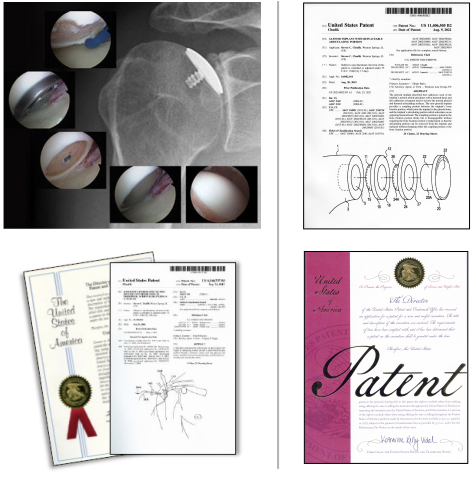
Innovations
US Patents and Patent Applications
- Method of Minimally Invasive Shoulder Replacement Surgery, U.S. Patent No. 9,445,910, filed September 11, 2006
- Humeral Implant for Minimally Invasive Shoulder Replacement Surgery. Patent application serial number 11/529,185 case II, filed September 25, 2006
- Glenoid Implant for Minimally Invasive Shoulder Replacement Surgery, U.S. Patent No. 9,974,658, filed September 25, 2006
- Humeral Implant for Minimally Invasive Shoulder Replacement Surgery, Serial No.11/525,629, filed September 25, 2006, application published as U.S. Patent App. Pub. 2007/0016305 (A)
- Guide for Shoulder Surgery, U.S. Patent No. 9,968,459, filed September 29, 2006
- Suture Pin Device. Patent application serial number 11/529,2006, case XV, filed September 29, 2006
- Suture Pin Device, Serial No. 11/529,185, filed September 29, 2006, application published as U.S. Patent App. Pub. 2007/0027477 (A)
- Method of Arthroscopic or Open Rotator Cuff Repair Using An Insertional Guide For Delivering a Suture Pin, U.S. Patent No. 8,540,737, filed October 24, 2006
- Acromioclavicular Joint Repair System, U.S. Patent No. 9,387,011, filed February 2, 2007
- Resurfacing Implant for a Humeral Head, Serial No. 13/068,309, filed May 9, 2011, application published as U.S. Patent App. Pub. 2012/0041563 (A)
- Universal Anterior Cruciate Ligament Repair and Reconstruction System(Cannulated Scalpel), U.S. Patent No. 10,034,674, filed February 2, 2007
- Resurfacing Implant for a Humeral Head. Patent application serial number 13/068,309 case II (A), filed May 9, 2011
- Method of Arthroscopic or Open Rotator Cuff Repair Using an Insertional Guide for Delivering a Suture Pin. U.S. Patent Number 8,540,737 B2, issued September 24, 2013
- Cortical Loop Fixation System for Ligament and Tendon Reconstruction, Serial No. 13/998,567, filed November 12, 2013, application published as U.S. Patent App. Pub. 2015/0134060 (A)
- Acromioclavicular Joint Repair System. U.S. Patent Number 9,387,011 B2, issued July 12, 2016
- Method of Minimally Invasive Shoulder Replacement Surgery. U.S. Patent Number 9,445,910 B2, issued September 20, 2016
- Guide for Shoulder Surgery. U.S. Patent Number 9,968,459 B2, issued May 15, 2018
- Glenoid Implant for Minimally Invasive Shoulder Replacement Surgery. U.S. Patent Number 9,974,658 B2, issued May 22, 2018
- Glenoid Implant with Replaceable Articulating Portion, U.S. Patent No. 11,406,505, filed August 20, 2019, issued August 9, 2022
- Cortical Loop Fixation Method for Ligament and Bone Reconstruction, Serial No. 15/731,719, filed July 24, 2017, application published as U.S. Patent App. Pub. 2019/0021845 (Pending)
- Humeral Implant and Method, Serial No. 17/532,714, filed November 22, 2021 (Pending), published as U.S. Patent App. Pub. US 2023/0157832
- Humeral Implant with Cannulation and Method, Serial No. 18/211,396, filed June 19, 2023 (Pending)
- Glenoid implant with Portal and Method, filed July 2023 (Pending)
Dr. Steven Chudik continually innovates to create new technology, and surgical techniques and improve patient care. He also collaborates worldwide with other leaders in the orthopaedic technology industry. Surgeries provide Dr. Chudik with an endless source of ideas to create new, safer, less invasive, and more effective surgical procedures, surgical instruments, and implants. Several of his shoulder patents are the direct result of these pioneering endeavors.
Research
An inquisitive nature was the impetus for Dr. Steven Chudik’s career as a fellowship-trained and board-certified orthopaedic surgeon, sports medicine physician, and arthroscopic pioneer for shoulder injuries. It also led him to design and patent special arthroscopic surgical procedures and instruments and create the Orthopaedic Surgery and Sports Medicine Teaching and Research Foundation (OTRF). Through OTRF, Dr. Chudik conducts unbiased orthopaedic research and provides up-to-date medical information to help prevent sports injuries. He also shares his expertise and passion for mentoring medical students in an honors research program and serving as a consultant and advisor for other orthopaedic physicians and industry.
Areas of Research And Development